What is a Dislocated Shoulder?
The shoulder is the most mobile joint in the body and thus susceptible to being dislocated or partially dislocated (aka subluxed). [1] The shoulder is classified as a ball and socket joint composed of three different bones: humerus, scapula and clavicle. Joints are classified as either stable joints, think knee (only moves in one direction) or a mobile joint like the shoulder or hip. Because of this mobility, stability of the joint is compromised and provided by not only the ligaments but also muscles known as the rotator cuff. These are the important dynamic restraints of the shoulder.
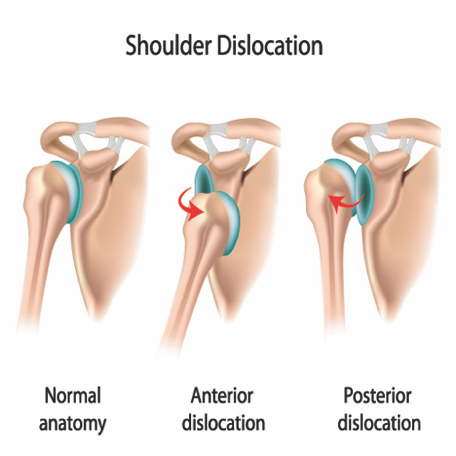
In the case of a shoulder dislocation, the ball (humerus) is forcefully put of out its position on its socket (glenoid labrum). This is typically associated with significant pain and an inability to use your arm until the shoulder is relocated. A shoulder subluxation is an instability event where the humerus will slide partly away from the glenoid labrum and return before a full dislocation occurs
Types of Dislocations
When the shoulder is dislocated from the joint it can occur in 3 different ways dependent upon the way that the humerus moves away from the glenoid.
· Anterior Dislocation – most common type accounting for 95-97% of cases caused by an arm being placed in a position of abduction and external rotation like making a tackle and the shoulder displaces forwards [2]
· Posterior Dislocation – accounts of approximately 2-4% of cases and occur with the humerus displaced towards the back of the body. This can occur with a fall on an outstretched arm or elbow [3]
· Inferior Dislocation – the rarest type where the top of the humerus is displaced downwards, typically occurs via trauma to the shoulder.
Causes
The most common cause of shoulder dislocation is trauma through force applied to the shoulder in various angles which causes the humerus to leave the glenoid labrum. These injuries commonly in contact sports such as Rugby and AFL, Eg. When making a tackle or when contact occurs contesting for a mark.
In addition, some people who have looser ligaments throughout their body who are able to dislocate their shoulder with relative ease. The best thing for this population is to do a targeted strengthening program to reduce the risk of dislocations occurring with repetitive shoulder movements. [4]
Management of Shoulder Dislocations
Once the shoulder is relocated, there are multiple factors that will determine which direction someone may choose to proceed with treatment. However normally non-operative rehabilitation is the first line of management. An assessment with a trained Sports Physio or Specialist Sports Doctor with the appropriate imaging can help decide the best course of management in each case.
Non-Operative Management
Conservative management is the first line of treatment in most cases of first time acute shoulder dislocation. The main goals in this type of management are
· Pain relief – reduce localised pain and reduce swelling (Rest Ice Compression Elevation - RICE)
· Physiotherapy - Maintain and restore muscular strength and proprioceptive feedback. Regain normal range of motion once pain has settled.
· Rehab - Increase strength to prevent further instability episodes and withstand the forces placed on the shoulder during sport and in daily life.
· Return to full function with prevention strategies to ideally avoid a recurrent dislocation
Surgical Management
Surgical management for this injury is common in recurrent dislocators and those returning to contact sports. These shoulder reconstructive surgeries are very successful in restoring stable anatomy allowing the athlete to their chosen sport competing at the same level. A sling will be applied post-surgery for a short period of time before the required physiotherapy. Strength rehabilitation is essential in restoring the shoulder to its pre-injury status and to prevent further injury. Rehab timeframes can last from 4-9 months depending on various factors.
Written By Sports Physiotherapist Simon Wybenga
References
1. Dodson, CC et al. Anterior glenohumeral hoint dislocations. Orthopaedic Clinical North America, 2008. 39(4): p507-18
2. Boone, JL et al. First time anterior shoulder dislocations: has the standard changed? British Journal of Sports Medicine, 2010. 44: p355-36
3. Farrar NG et al. An overview of shoulder instability and its management. Open Orthopaedic Journal, 2013. 7: p338-346
4. Cutts, S et al. Anterior shoulder dislocation. Ann R Coll Surg England, 2009. 91(1): p2-7
5. Wang, RY et al. The recognition and treatment of first-time shoulder dislocation in active individuals. JOSPT, 2009. 39(2):p118-123